Is your practice leaving money on the table, or worse, inviting a RAC audit? MedBill RCM Solutions provides deep-dive medical billing audits designed to identify “leakage” in your revenue cycle and ensure your documentation stands up to payer scrutiny. Our experts bridge the gap between clinical care and financial integrity, providing you with a roadmap to 100% billing accuracy and maximized reimbursements.

We meticulously analyze your claims data to find under-coded services, missed modifiers, and unbilled procedures. This recovery-focused approach ensures you receive every cent of the reimbursement you are legally entitled to.
Our auditors review your charts against CMS and OIG guidelines to identify “red flags” like over-coding or cloning. By catching these issues internally, we protect your practice from heavy fines and federal audits.
We don’t just find errors; we find their source. Our audits pinpoint bottlenecks in your staff’s workflow, allowing us to recommend training and technology fixes that prevent future billing mistakes.
Our auditing suite is designed to address specific pain points within your revenue cycle. These specialized reviews ensure that your billing is both optimized for revenue and fortified against audits.
We perform high-level reviews for hospital-based services to ensure that Diagnosis Related Groups (DRG) are assigned correctly, preventing costly "down-coding" by payers.
We analyze your Evaluation and Management (E/M) coding distribution to ensure you aren't "under-coding" out of fear or "over-coding" in a way that triggers insurance red flags.
This focused audit investigates your highest-volume denial reasons to determine if the issue lies in registration, coding, or payer-specific "hidden rules."
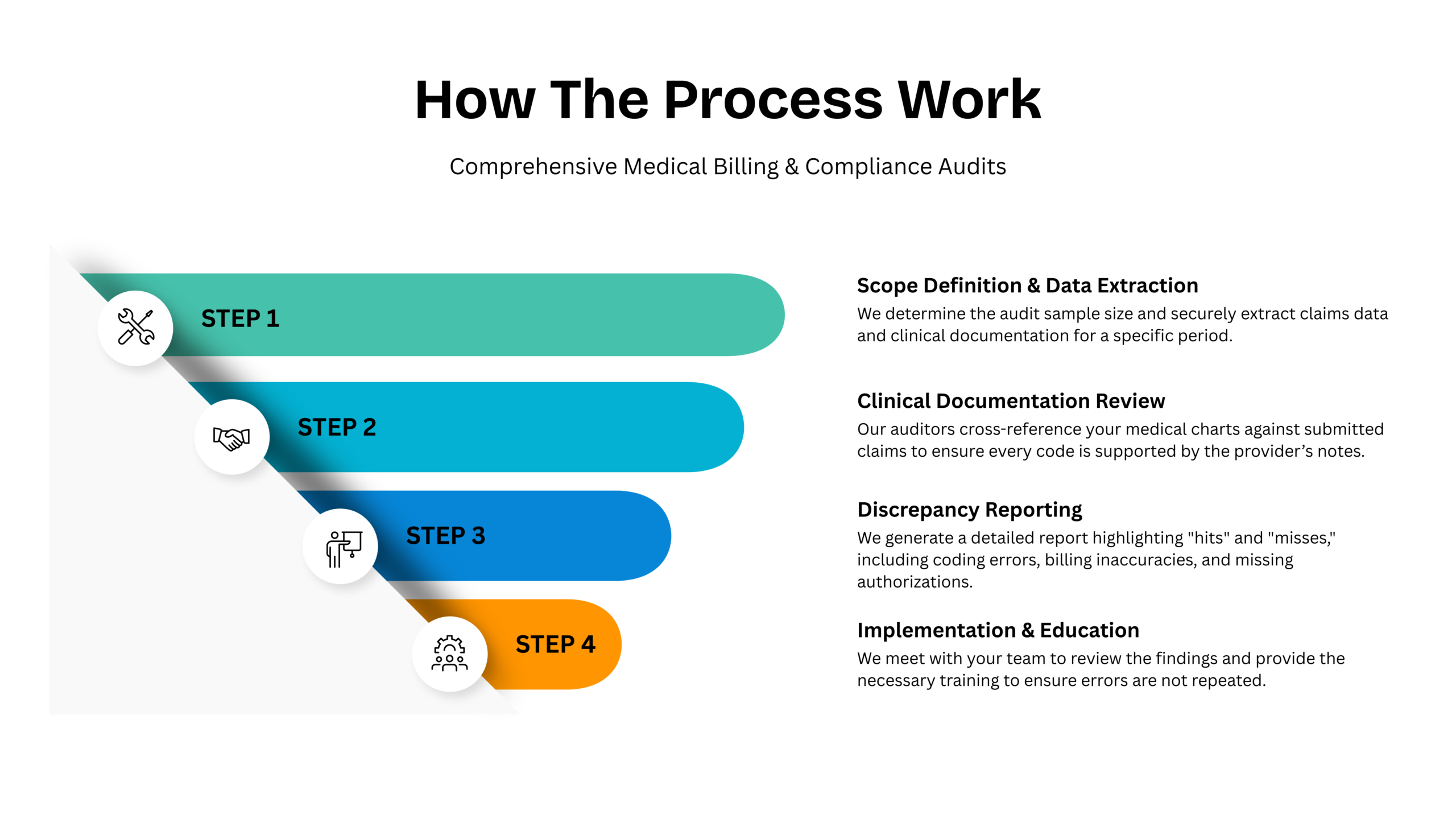
Our auditing methodology is rigorous, transparent, and designed to provide a 360-degree view of your billing health. We turn complex data into a simple, actionable plan for growth.
We determine the audit sample size and securely extract claims data and clinical documentation for a specific period.
Our auditors cross-reference your medical charts against submitted claims to ensure every code is supported by the provider’s notes.
We meet with your team to review the findings and provide the necessary training to ensure errors are not repeated.

Ensuring that your needs are met with precision and attention to detail.

Our dedicated account managers are available around the clock to assist your team with urgent verification or registration hurdles.


MD | Sterling Family Medicine
"Saved Us from a Compliance Nightmare" "The audit from MedBill RCM Solutions uncovered coding errors we didn't even know we were making. They helped us fix the issues before they became a problem with Medicare."

Clinic Director
"Uncovered 15% in Lost Revenue" "We thought our in-house billing was fine until MedBill did an audit. They found thousands in missed modifiers and unbilled services. The audit paid for itself in the first month."