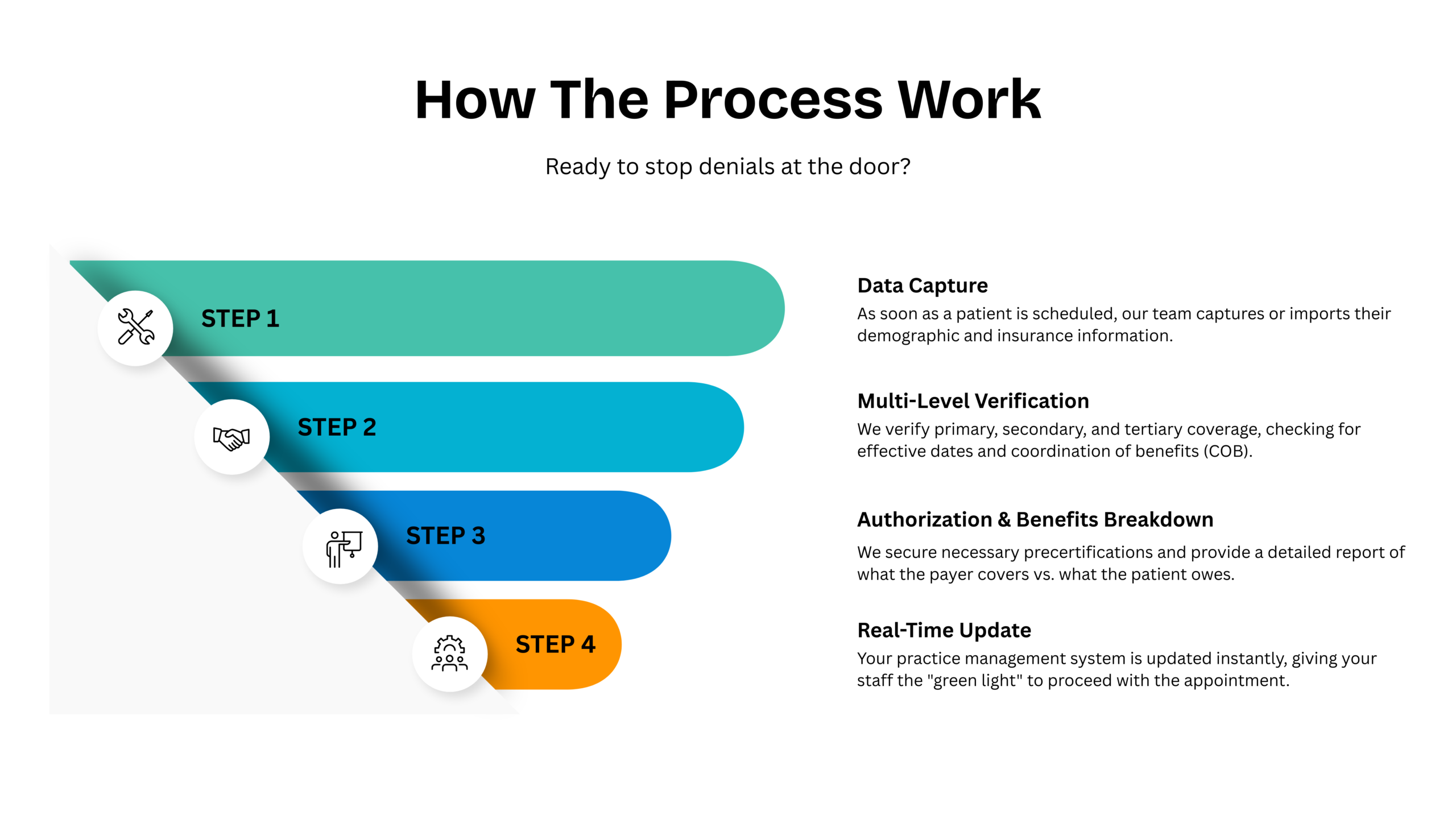
At MedBill RCM Solutions, we know that a clean claim begins the moment a patient schedules an appointment. Our expert verification services eliminate the administrative errors that cause 25% of all medical billing denials. By validating coverage and securing authorizations upfront, we ensure your practice has a solid financial foundation for every patient encounter.

We instantly validate insurance status and benefit details to ensure coverage is active before the patient encounter. This proactive check eliminates “Member Not Found” rejections and ensures you only treat covered patients.
Our dedicated team manages the complex communication with payers to secure necessary approvals before procedures are performed. By handling the paperwork and follow-ups, we prevent costly denials for unauthorized medical services.
We calculate exact co-pays, co-insurance, and remaining deductibles to provide total financial transparency for your patients. This empowers your front-desk staff to collect payments confidently at the point of care, significantly boosting your cash flow.
Beyond basic data entry, MedBill RCM Solutions provides specialized support to manage the most complex hurdles in the registration process. Our subservices are designed to eliminate bottlenecks and ensure your claims are “clean” before they ever reach a coder.
Navigating payer portals and clinical requirements is a full-time job that we handle for you. We manage the entire lifecycle of authorizations, ensuring every procedure is pre-approved and documented to prevent retrospective denials.
We determine the correct payer order for patients with multiple insurance plans to prevent payment delays. Our team proactively resolves conflicts between primary and secondary insurers, so your claims aren't "pended" for months.
Our team performs a rigorous scrub of patient records to correct errors in addresses, social security numbers, and insurance IDs. By ensuring data integrity at the start, we prevent the "Return to Provider" rejections that stall your cash flow.
Most billing failures happen at the front desk. MedBill RCM Solutions acts as your proactive gatekeeper.
We meticulously audit patient demographics to prevent "Return to Provider" rejections.
Free your staff from hour-long hold times with insurance companies; we handle the calls for you.
Provide clear, accurate cost estimates upfront, reducing billing disputes and increasing patient satisfaction.

Ensuring that your needs are met with precision and attention to detail.

Our dedicated account managers are available around the clock to assist your team with urgent verification or registration hurdles.


MD | Sterling Family Medicine
The Gold Standard for Front-End Accuracy" "Before partnering with MedBill RCM Solutions, our practice was plagued by 'Patient Not Eligible' denials that ate into our monthly revenue. Since they took over our verification process, those denials have dropped to nearly zero, and our front-desk staff can finally focus on patient care instead of fighting with insurance companies.

Clinic Director
Transformed Our Cash Flow" "The ability to know exactly what a patient owes before they even walk in has been a game-changer for us. MedBill’s accurate responsibility estimates allowed us to increase our point-of-service collections by 40%. They are truly a partner in our financial success.

DO
Authorization Headaches Are Gone" "Securing prior authorizations used to be a full-time job for two of my employees. MedBill RCM Solutions stepped in and streamlined the entire workflow. Their team is fast, efficient, and they never miss a detail. I can’t imagine running our surgical center without their support.